![]()
My Death, My Decision’s Campaigns and Communication Manager, Keiron McCabe, responds to the latest Guardian long-read “Death on demand: has euthanasia gone too far?”
Christopher Bellaigue raises an important question for those of us who advocate for assisted dying reform. In a society which permits euthanasia, what are the acceptable limits to autonomy? As the Netherlands has demonstrated, this question yields no easy answers, and its answer will differ depending upon one’s moral, social and religious background. Yet whilst Bellaigue is right to have raised such an important question, he is wrong to have drawn such a quick conclusion.
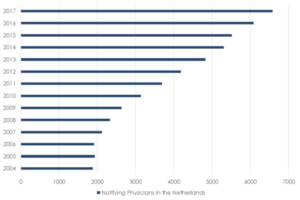
Bellaigue presents a bleak picture of the Netherlands. Drawing upon a declining rate of euthanasia, he connects the “long-term consequences” of Euthanasia, and a lack of resolve and “willingness” from doctors, to suggest the country now “doubts” its decision to legalise assistance to die. Paradoxically, he also writes about a rising rate of Euthanasia, and that “in 2017, some 1,900 Dutch people killed themselves”. The implication being that euthanasia “cheapen[s] life itself”, and encourages higher levels of suicide. Leaving aside these paradoxes, these connections are misleading. Since 2004, there has been a 249% increase in the number of notifying physicians, involved in Euthanasia and the Dutch suicide rate remains at about the same level as it was before the law changed.
Bellaigue also suggests that in 2002 the Netherlands should have “stipulate[d] that patients must be competent at the time” they make a decision to end their life. The importance of this requirement is abundantly clear in the context of Dementia, as Bellaigue raises, because it is only in the early-stages of Dementia that someone can retain the capacity to make an autonomous decision. Yet, it is misleading to suggest that competence is unnecessary, at the time of death, in the Netherlands. Whilst the requirement of “competence” may not be clear upon first inspection, since the 2002 law does not explicitly use the term, the 2018 Dutch Euthanasia code is clear that mental competence is encapsulated within the legal requirement for a patient to make a “voluntary and well-considered request”.
At no point is Bellaigue’s warning clearer, than his concern that euthanasia is leading to “death on demand”, a conception which incidentally had been discussed since 2010 but never realised. Few advocates of a right to die, condone an entirely unencumbered entitlement. Most would argue, as I would, that alongside any right to a die, there must be a stringent and robust set of safeguards to protect those who are most vulnerable. Determining the limits of that right is a difficult task. For some, assistance may turn upon the presence of a terminal illness; whilst for others, the permission of a loved one may be essential.
I believe that the answer lies in empowering mentally competent adults, who suffer from incurable health problems, with the freedom to determine the course of their own lives. It is our ability to act autonomously which gives life meaning. Both in the sense of taking responsibility for our actions, and in owning our individual destinies. When an incurable illness robs someone of that ability, and their quality of life falls permanently below a level that they find can acceptable, it is wrong to force them to live against their will.
Euthanasia is a complex and difficult question, which demands a sensitive and careful discussion. It is incumbent upon us all to make sure we hold ourselves to that standard.

