
Subject: Oral Evidence Sessions: Day 2 Session 2 Legal and Palliative Care Considerations
This afternoon saw the second session of the second day of oral evidence. The Committee examining the Terminally Ill Adults Bill questioned experts on the legal aspects of the Bill, as well as the palliative care and disability considerations.
Make sure to read our summary of yesterday’s morning session and afternoon session, and this morning’s session.
Session 1:
The first session included four experts in a range of medical professions, elderly care and assisted dying expertise:
- Dr Alexandra Mullock, University of Manchester
- Professor Allan House, University of Leeds
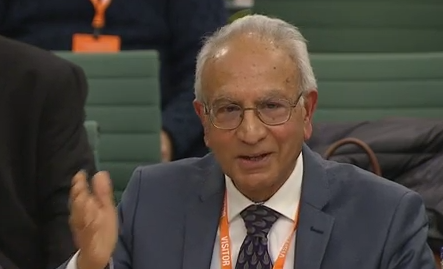
- Professor Aneez Esmail, University of Manchester
- Richard Robinson, CEO, Hourglass
Richard Robinson, CEO of Hourglass, a specialist organisation focusing exclusively on issues relating to the abuse of older people, told the committee that elderly people can be very vulnerable, but that notion of vulnerability only extends to a small proportion of older people. He told the committee:
“Older people deserve the same independence and autonomy as every other demographic. Not all older people are vulnerable.”
Professor Aneez Esmail, talked about the shortfalls in the current legal framework:
“At the moment people go sooner than they would wish to die because they have to go to Switzerland while they’re still well enough to travel and they also have this terrible fear that their loved ones will be then prosecuted by the police.
This creates huge amounts of stress and is really unpleasant… having a system of perspective rather than a retrospective assessment of the person when it’s too late after they’ve died will be absolutely a better approach – more compassionate and provide better safeguards than what we have at the moment.”
Dr Alexandra Mullock was asked about citizens’ juries that she played a role in Jersey, as well as the Nuffield Council of Bioethics’s citizen jury. She said:
“Both juries went through a huge amount of evidence that was very balanced in terms of being pro-and anti-assisted dying, I think it’s fair to say …the majority of people as they became more informed… they stayed quite true to their initial beliefs.”
Session 2:
The second session saw a range of experts with different specialities around law, human rights and disability.
- Dr Lewis Graham (University of Cambridge),
- Baroness Falkner, chair of the Equality and Human Rights Commission (EHRC)
- Lord Sumption, Lord Justice at the Supreme Court
- Fazilet Hadi, Head of Policy at Disability Rights UK
Lord Sumption, Former Justice of the Supreme Court of the United Kingdom, told the Committee that the current provision for the High Court to look at all assisted dying cases is ‘over-engineered’, “unnecessary’ and ‘undesirable’.
Speaking today on the second day of the evidence session for the Terminally Ill Adults (End of Life) Bill Committee, Lord Sumption told MPs:
“My own view is that clause 12 is unnecessary and in some respect undesirable. I’ve seen the proposed amendment relating to a panel which would resolve the problem of the shortage of capacity in the High Court, but it would not resolve the problem of the over-engineering of the procedural provisions of this Bill.”
Clause 12 relates to a current provision in the Bill that outlines that all assisted deaths would require the sign-off of a High-Court judge. No other jurisdiction in the world that allows assisted dying requires the approval of a judiciary. He continued:
“It is not entirely clear what the judge is supposed to do. There are many things that he is entitled to do. But, the real question is: ‘is he there to ensure that the two doctors have done their job and the ducks are all there in a row, or is he there to form his own view on all of these matters, completely independently of all those who have given their certificates?’ If the latter, one is talking about quite a time-consuming process, involving a lot of additional evidence. It seems to me this is a protection which no other country so far that I am aware of among those who have authorised assisted dying have included.
I think it infers a protection that is largely illusory and undoubtedly very time-consuming. I have a residual feeling, that you could fairly describe as a prejudice, that it involves the intervention of the state in an intensely personal agonising process, which to my mind is inappropriate.”
Talking about the European Convention on Human Rights, and whether the proposed legislation would be compatible, Dr Lewis Graham explained that the European Court of Human Rights in Strasbourg found that the Belgian assisted dying law is compatible and that the Terminally Ill Adults Bill in the UK has even greater protections, and therefore would surely be compatible.
Dr Graham explained that UK Courts have made it very clear that assisted dying is a matter for Parliament, and any changes or challenges to the law would likely need to go back to Parliament.
Fazilet Hadi and Baroness Falkner both raised concerns with the Private Members’ Bill process, arguing that much more scrutiny and consultation would have happened under a government Bill. Hadi raised the concerns of some disabled people, saying:
“Disabled people are not a homogenous group. It isn’t about counting how many people are supportive and not supportive… It’s about how equality works and the barriers we face.“
Session 3:
- Toby Porter, CEO of Hospice UK,
- Dr Jamilla Hussain, Bradford Teaching Hospitals NHS Trust and Hull York Medical School
- Dr Jane Neerkin, Consultant Physician in Palliative Medicine
- Sam Royston, Executive Director of Policy and Research at Marie Curie.
This session has a strong focus on palliative care, and the provision of palliative care. Similar to the session during the Health and Social Care Committee’s inquiry into assisted dying, there was a hyper-focus on what changes need to be made to the palliative care sector, which occasionally moved away from scrutinising the Terminally Ill Adults Bill.
Asked about eligibility, Dr Hussain said:
“Usually, the decision is not related to symptoms, it’s related to control being really important. I’m not personally in principle against assisted dying, I think it’s quite distressing, when control is important, to not feel you have it.
The other side of it is people much closer to end of life, who perhaps have had a long trajectory, they are in the last few weeks, perhaps their symptoms aren’t best controlled as they want to be or they are just fed up and their family have got to that stage. And for that I don’t think this Bill is fit for purpose. I think the length of time it would take to go through the Bill would mean that they wouldn’t be eligible.”
Dr Neekin said:
“I think first of all death and dying is not owned by palliative care and I think we’re hearing a lot about palliative care but you know we’ve also heard from GPs that they deal with a lot of death and dying as does every other speciality.
So first of all we don’t own death and dying and I think a lot is being put on palliative care first of all and I also think that palliative care is not a panacea for everything at the end of life.“
Both Porter and Royston outlined the issues the palliative care sector is currently facing, but both organisations take a neutral stance on assisted dying. When suggesting specific amendments, Royston outlined that there was an assessment of the provision of palliative care five years after legalisation, but not at the start.
Claire Macdonald, Director of My Death, My Decision says:
“MPs have heard a range of evidence today. We are glad to be reassured that the Bill is safe and workable. However, there’s more and more evidence that we may be making a law that is too cumbersome and difficult to navigate, and eligibility may be too strict.
People who are dying and people who are suffering want choice and dignity at the end of their lives – it’s the duty of politicians to make this legislation safe, compassionate and workable.”
Introduced by the Labour MP Kim Leadbeater MBE, the Bill will allow adults who are terminally ill with six months or fewer left to live to ask for help to end their own lives. In November, MPs voted on the principle of this legislation, passing the second reading 330 votes to 275. The Bill is currently in the Committee Stage, where it will remain for several months of scrutiny before a final vote in the House of Commons next year.
The Bill applies to England and Wales only. A private member’s bill in Scotland by Liam McArthur MSP has been introduced in the Scottish Parliament.
Notes:
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033.
Media can use the following press images and videos, as long as they are attributed to “My Death, My Decision”.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow mentally competent adults who are terminally ill or intolerably suffering from an incurable condition the option of a legal, safe, and compassionate assisted death. With the support of over 3,000 members and supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give the people of England and Wales choice at the end of their lives.




 All three experts told the Committee how the Australian states have safe, compassionate and working assisted dying laws. Dr Mewett told the committee:
All three experts told the Committee how the Australian states have safe, compassionate and working assisted dying laws. Dr Mewett told the committee: Citing his quality research with disabled people, Professor Tom Shakespeare, told the Committee:
Citing his quality research with disabled people, Professor Tom Shakespeare, told the Committee: Citing his 20 years of human rights work, Yogi Amin told the committee:
Citing his 20 years of human rights work, Yogi Amin told the committee: 
 Dr Sam Ahmedzai said:
Dr Sam Ahmedzai said: Sir Nicholas Mostyn told MPs that he may still have to go to Dignitas, even if the Bill passes. He told MPs:
Sir Nicholas Mostyn told MPs that he may still have to go to Dignitas, even if the Bill passes. He told MPs: On concerns about coercion, Dr Ryan Spielvogal, Senior Medical Director for Aid in Dying Services in California, told MPs:
On concerns about coercion, Dr Ryan Spielvogal, Senior Medical Director for Aid in Dying Services in California, told MPs:
 Sir Chris Whitty, the Chief Medical Officer for England, told the Committee examining assisted dying legislation that “It’s important that the wishes of the patient must be respected, we must think about the wishes of someone in the last six months of their life and their family”.
Sir Chris Whitty, the Chief Medical Officer for England, told the Committee examining assisted dying legislation that “It’s important that the wishes of the patient must be respected, we must think about the wishes of someone in the last six months of their life and their family”. Dr Andrew Green, Chair was asked if doctors should be prohibited from talking about assisted dying to their patients. He replied: “Please do not pass legislation that makes it harder for doctors to understand their patients.”
Dr Andrew Green, Chair was asked if doctors should be prohibited from talking about assisted dying to their patients. He replied: “Please do not pass legislation that makes it harder for doctors to understand their patients.” Professor Nicola said the role of a nurse is to listen and advocate for the patient:
Professor Nicola said the role of a nurse is to listen and advocate for the patient: 





 MPs have
MPs have 
 A representative from DIGNITAS has told MPs that assisted dying at the Swiss centre is “safe, peaceful and compassionate” for the people who end their lives there. Silvan Luley, a representative of ‘DIGNITAS – to live with dignity, die with dignity’, spoke to politicians at a closed-room briefing organised by My Death, My Decision.
A representative from DIGNITAS has told MPs that assisted dying at the Swiss centre is “safe, peaceful and compassionate” for the people who end their lives there. Silvan Luley, a representative of ‘DIGNITAS – to live with dignity, die with dignity’, spoke to politicians at a closed-room briefing organised by My Death, My Decision. Clare Turner, a mum of two from Devon who has stage 4 breast cancer, rescheduled her chemotherapy treatments to talk to MPs. Clare said:
Clare Turner, a mum of two from Devon who has stage 4 breast cancer, rescheduled her chemotherapy treatments to talk to MPs. Clare said:



Recent Comments