
This afternoon, the Committee which is examining the Terminally Ill Adults Bill, heard evidence from palliative care, and legal and international experts.
Our summary of the morning session is available here, but here is our summary of the afternoon session:
Session 1:
- Dr Rachel Clark, Palliative Care doctor
- Dr Sam Ahmedzai, Emeritus Professor at the University of Sheffield
- James Sanderson, CEO of Sue Ryder,
- Dr Sarah Cox, President of Association of Palliative Medicine
This session saw a range of reviews looking at the state of palliative care in the UK and whether individuals can make an informed decision about assisted dying if there’s not currently uniform equality of access.
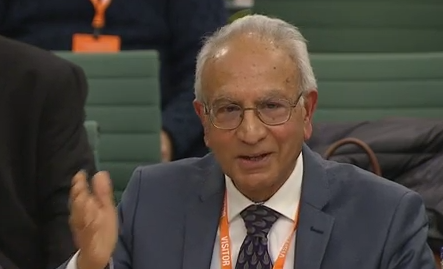 Dr Sam Ahmedzai said:
Dr Sam Ahmedzai said:
“British people have had that option for many years since Switzerland offered it. It’s clear, it’s selecting our people who are better off, and more functionally capable. They can do that, so it discriminates against disabled people who go long before they need to. They need to because they mostly want to go on their own without dragging relatives along so it’s doubly damaging for families because they have to say goodbye long before they have to do that.”
Dr Rachel Clark told MPs:
“If there is one thing that I would say to the Committee about making the bill as robust and strong and safe as possible. Please consider seriously the matter of education and training from day one of medical school and onwards. Death is at the periphery of a medical school curriculum, you might get a week of palliative care in five years”
James Sanderson said:
“Increasingly hospices are reading beyond the walls of the hospice into the community, people want to die at home, supporting people at home enables us to go out into the community.”
Dr Sarah Cox said:
“I accept there will be people even with a very good palliative care system who will still choose assisted dying. We currently don’t have the palliative care system that we need and that’s what concerns me.”
Session 2:
- Sir Max Hill KC,
- Alex Ruck Keene KC (Hon),
- Sir Nicholas Mostyn
Sir Max Hill told MPs that in his experience of working as Director of Public Prosecutions, he oversaw a number of cases to do with people travelling to Dignitas. He told MPs
“In each of the 27 cases I considered the deceased individual was already dead and that is when the scrutiny started. A major advantage of this Bill is that would be reversed and scrutiny would be before death.”
 Sir Nicholas Mostyn told MPs that he may still have to go to Dignitas, even if the Bill passes. He told MPs:
Sir Nicholas Mostyn told MPs that he may still have to go to Dignitas, even if the Bill passes. He told MPs:
“I fear that I am one of the people who has to go to Dignitas, and frankly I can afford to do that, because this bill is never going to provide an assisted death for me.
I’m not going to be graphic about what the advanced stages of Parkinson’s are like, but the medical members amongst you will be able to describe what is likely, not definitely, but likely to await me. It is either going to be a poor death here, or to go somewhere like Dignitas. I would be very surprised, if my children drove me to Calais, and then drove me onto Zurich, I would be very surprised if any prosecution ensued…”
A large part of the session focused on the legal aspects of the Bill, including if it could be challenged in the courts.
Alex Ruck Keene KC said:
“We get into this enormous argument about “is it inevitably discriminatory?”, and courts today have been very clear we are not going to get into it, it’s for parliament to decide whether or not to make assisted dying legal.”
“Once it has been made legal for some but not others, there’s a difference in treatment. Whether it is discriminatory, and contrary to an article in the ECHR, depends on whether that difference is justified.
Parliament needs to be very very clear why, if you’re going to limit this, why it could be explained to somebody that you are not eligible and that it is a difference in treatment but it is perfectly justified.”
The session also went into depth about the current clause in the Bill that mandates the patient seek approval from the High Court. Committee members pressed the experts on whether other potential systems were workable, such as panels and tribunals.
Session 3:
- Dr Ryan Spielvogal (Senior Medical Director for Aid in Dying Services, Sutter Health, USA),
- Dr Jessica Kaan (Medical Director, End of Life Washington)
 On concerns about coercion, Dr Ryan Spielvogal, Senior Medical Director for Aid in Dying Services in California, told MPs:
On concerns about coercion, Dr Ryan Spielvogal, Senior Medical Director for Aid in Dying Services in California, told MPs:
“I’ll tell you in practice it just doesn’t happen. So I’ve seen assisted dying laws go into practice across numerous states. I have helped many many people through this process, I have never seen a case of even suspected coercion.
People are just not that good as actors. We get the family out of the room, we dig deep into their concerns and their justifications and reasoning behind their choices. It is often extremely crystal clear. They are focused on their quality of life, they are focused on their suffering.
‘I don’t ever get the sense from them, the family, or doctors, or anyone are coercing them into a decision. If anything, I’ve seen it many times the other way around. The patient is ready to let go but the family is not ready to let go, and they put various degrees of roadblocks to the patient accessing it.”
Dr Jessica Kaan, Medical Director of End of Life Washington, reinforced these claims. She told MPs:
“I would echo those comments. We are trained to assess capacity in big ways and small ways, throughout our medical training.
‘Virtually all of the time it is the opposite way around, where the family are trying to coerce or convince someone not to make this choice… I have also never come across a case where I felt a patient was being coerced into this decision by a family member.”
Claire Macdonald, Director of My Death, My Decision says:
“It was very reassuring to hear from the American doctors who work extensively on assisted dying that the work they do is rewarding – and that they have no concerns over coercion. They also stressed that doctors should freely be able to discuss assisted dying with patients and their families”.
What’s Next:
This was the second oral evidence session of the day. These evidence sessions will continue throughout Wednesday and Thursday, then followed by line-by-line scrutiny of the Bill, where a committee of MPs will look at the details and suggest changes.
Introduced by the Labour MP Kim Leadbeater MBE, the Bill will allow adults who are terminally ill with six months or fewer left to live to ask for help to end their own lives. In November, MPs voted on the principle of this legislation, passing the second reaching 330 votes to 275.
The Bill applies to England and Wales only. A private member’s bill in Scotland by Liam McArthur MSP has been introduced in the Scottish Parliament.
Notes:
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033.
Media can use the following press images and videos, as long as they are attributed to “My Death, My Decision”.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow mentally competent adults who are terminally ill or intolerably suffering from an incurable condition the option of a legal, safe, and compassionate assisted death. With the support of over 3,000 members and supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give the people of England and Wales choice at the end of their lives.

